
We should stop remembering the H’s & T’s of PEA and instead look for the most common reversible causes with the use of POCUS.We don’t really have outcomes data with this and may never have outcomes data either Cardiac Arrest Sonographic Assessment (CASA): Use a phased array probe in the subxiphoid view to look for: Pericardial Effusion, Right Heart Strain, and then Cardiac Activity.Delegate someone to count out loud to limit time off the chest doing CPR.If you don’t feel a pulse in profound shock your reflexive action is to resume CPR and give 1mg epinephrine, which may not be beneficial.Your Digitometer (Your Fingers) have a very low sensitivity at picking up pulses in profound shock.A quick summary of their thoughts are written below. Pseudo-PEA would benefit from pressor support as well, but use of POCUS should not delay high-quality CPR, and should not be used in isolation to determine whether to continue resuscitation efforts.Īfter Swami and I’s recording I was able to sit down with Joe Bellezzo and Scott Weingart to pick their brains about pulse checks, POCUS causing delays in CPR, 2 types of PEA, ECMO, and TEE. The presence of cardiac activity in PEA patients may encourage more aggressive resuscitation.”Ĭlinical Take Home Point: POCUS is an important tool in distinguishing pseudo-PEA (aka profound shock) from true-PEA, as differentiating having a pulse vs not having a pulse is difficult using palpation alone. This may be due to the inaccuracy of a single subcostal view, but this needs to be balanced as time doing ultrasound is time away from the things that matter for patients, high-quality CPR with limited interruptions.Īuthor Conclusion: “In cardiac arrest patients who present with PEA, bedside US has an important role in predicting ROSC. parasternal long axis, apical 4 chamber view, etc) was associated with ROSC in PEA. Finally, US evaluation results were not blinded to providers performing them which adds an additional layer of bias in whether to continue or terminate resuscitation efforts.ĭiscussion: Interestingly, in their meta-analysis, the authors found that using just a subxiphoid view only was not associated with ROSC in PEA arrest, but using various other views (i.e. Another issue with this study is that, definitions of ROSC and “cardiac motion” on ultrasound were not consistent between studies adding to the heterogeneity. RR 4.35 95% CI 2.20 – 8.63 p 40% of the patients included in this meta-analysis were from two studies, the other nine studies were all small trials.PEA Cardiac Arrest Patients Achieving ROSC:.Of the patients who achieved ROSC (81.7%), 188 of them had US identified cardiac activity (Pseudo PEA). 11 studies with 777 PEA patients were included in this analysis, with 230 patients achieving ROSC.Cardiac US performed during resuscitation.

Outcomes: The major primary outcome was ROSC in this study. What They Did: This was a systematic review and meta-analysis of studies that used US to predict ROSC

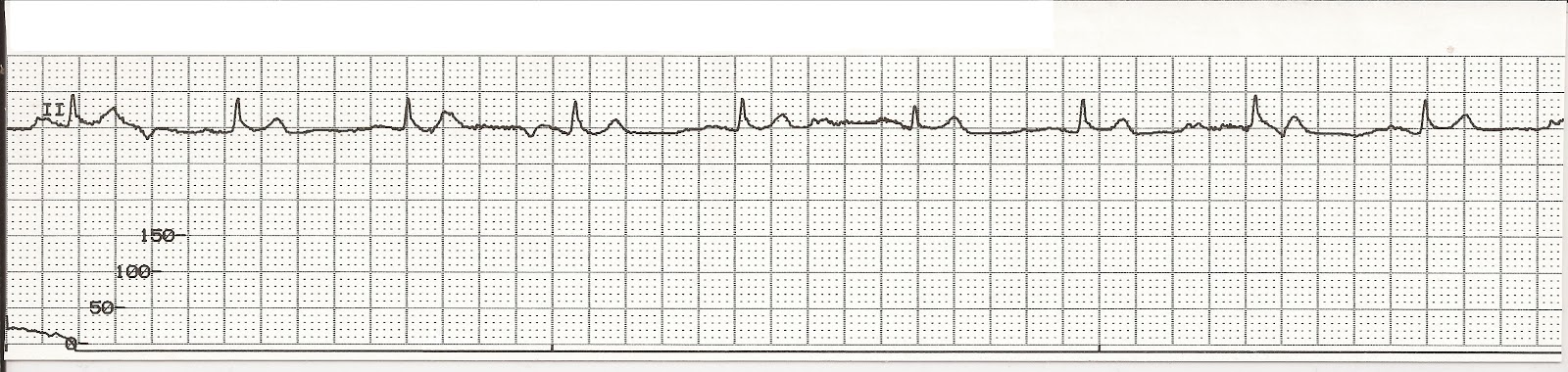
PEA PULSELESS ELECTRICAL ACTIVITY EKG DOWNLOAD
Click here for Direct Download of Podcast


 0 kommentar(er)
0 kommentar(er)
